Summary: Key Takeaways on Branchial Cleft Cysts
- Congenital origin, most commonly from the second branchial cleft.
- Typically presents as a painless neck mass in children or young adults.
- MRI and ultrasound are first-line imaging tools.
- Important to distinguish from other cystic neck lesions, including malignancies.
Understanding the imaging features and differential diagnoses of BCCs can significantly improve patient outcomes and reduce diagnostic delays.
What Is a Branchial Cleft Cyst? A Radiologist’s Guide to Diagnosis and Imaging
Branchial cleft cysts (BCCs) are a common congenital neck mass found primarily in children and young adults, though they can present at any age. These benign cysts arise from incomplete obliteration of the branchial apparatus during embryologic development and are often discovered incidentally during imaging for other complaints—or when they become infected or enlarged.
In this blog, we’ll answer common questions about branchial cleft cysts, including how to identify them, differentiate them from other neck masses, and optimize your imaging approach. Whether you're a radiologist in training or a seasoned practitioner, understanding BCCs is key to accurate diagnosis and appropriate management.
Explore diagnostic cases and imaging examples of Branchial Cleft Cysts on our BCC diagnosis page.
What is a Branchial Cleft Cyst?
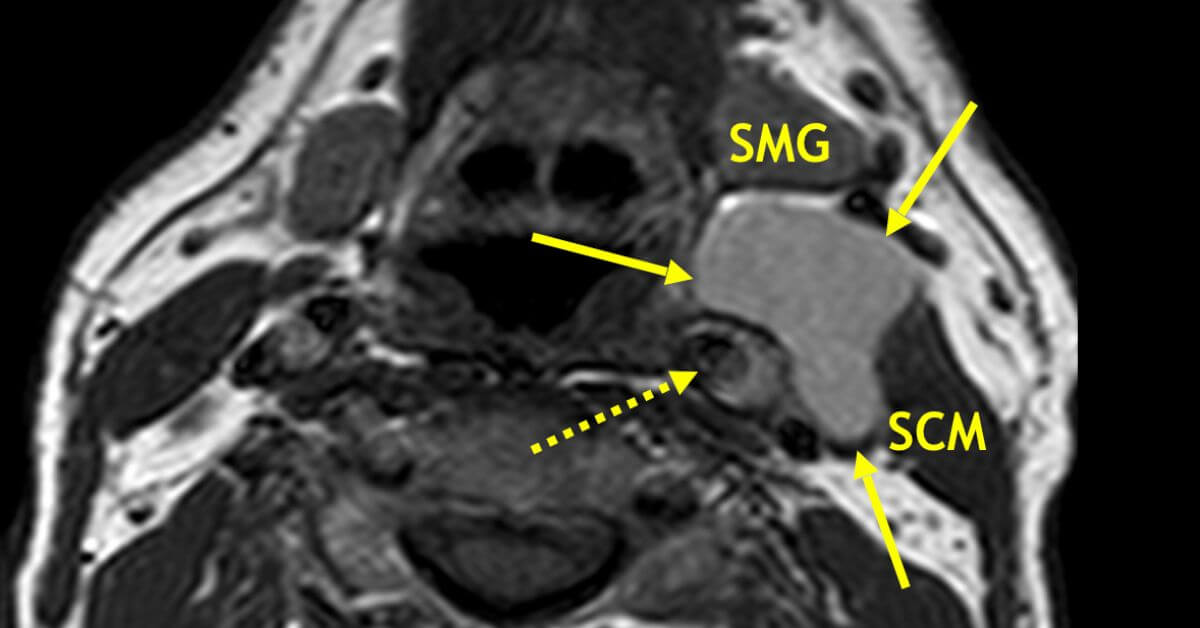
A branchial cleft cyst is a congenital epithelial cyst that forms due to the incomplete involution of the branchial apparatus, typically from the second branchial cleft. These cysts are usually located along the anterior border of the sternocleidomastoid muscle and can range in size from small and asymptomatic to large, compressive, or infected.
Key Imaging Features of Branchial Cleft Cysts
Modality of Choice:
- MRI is often the preferred modality, particularly when evaluating the extent and relation to adjacent structures.
- Ultrasound is useful for initial evaluation in pediatric patients.
- CT may be used to better delineate anatomy, especially pre-operatively or in the presence of infection.
MRI Findings:
- Well-circumscribed, non-enhancing cystic mass with high T2 signal intensity.
- Homogeneous fluid content unless infected (may show rim enhancement or internal debris).
- Location is key: most second branchial cleft cysts are found near the angle of the mandible or adjacent to the carotid space.
View sample BCC imaging cases and MRI findings on our Branchial Cleft Cyst diagnosis page.
Types of Branchial Cleft Cysts
There are four main types of BCCs based on the branchial cleft of origin:
- First Branchial Cleft Cyst – Typically near the external auditory canal or parotid gland.
- Second Branchial Cleft Cyst – Most common; located along the anterior border of the sternocleidomastoid.
- Third and Fourth Branchial Cleft Cysts – Rare; may extend into the lower neck or mediastinum.
Differential Diagnosis
Because BCCs are often painless and slowly enlarging, it’s crucial to differentiate them from other neck masses. Consider:
- Thyroglossal duct cysts
- Lymphangiomas
- Cystic metastases, especially in adults
- Abscesses or infected lymph nodes
- Dermoid/epidermoid cysts
Imaging and clinical history are essential to make the distinction. In adult patients, especially with atypical features or rapid growth, malignancy must be ruled out.
When to Suspect a Branchial Cleft Cyst?
Radiologists should consider BCC in cases where:
- A young patient presents with a painless, lateral neck mass.
- Imaging reveals a well-circumscribed cyst without solid components.
- The lesion is located in a predictable anatomic location (e.g., near the carotid space or mandible).
Learn More and Review Diagnostic Cases
At Medality, we help radiologists and trainees sharpen their diagnostic accuracy with real-world cases and expert-led reviews. Our Branchial Cleft Cyst diagnosis page includes:
- Clinical imaging examples
- Case-based learning
- Tips for identifying BCCs on MRI and other modalities