Summary: Key Takeaways on Encephalomalacia
- Encephalomalacia is the end result of liquefactive necrosis in the brain, commonly caused by infarction, hemorrhage, or trauma.
- It can occur in any age group and location, with the anteroinferior frontal and temporal lobes often affected after trauma.
- Lesions may be asymptomatic or lead to neurologic deficits or seizures, depending on their location.
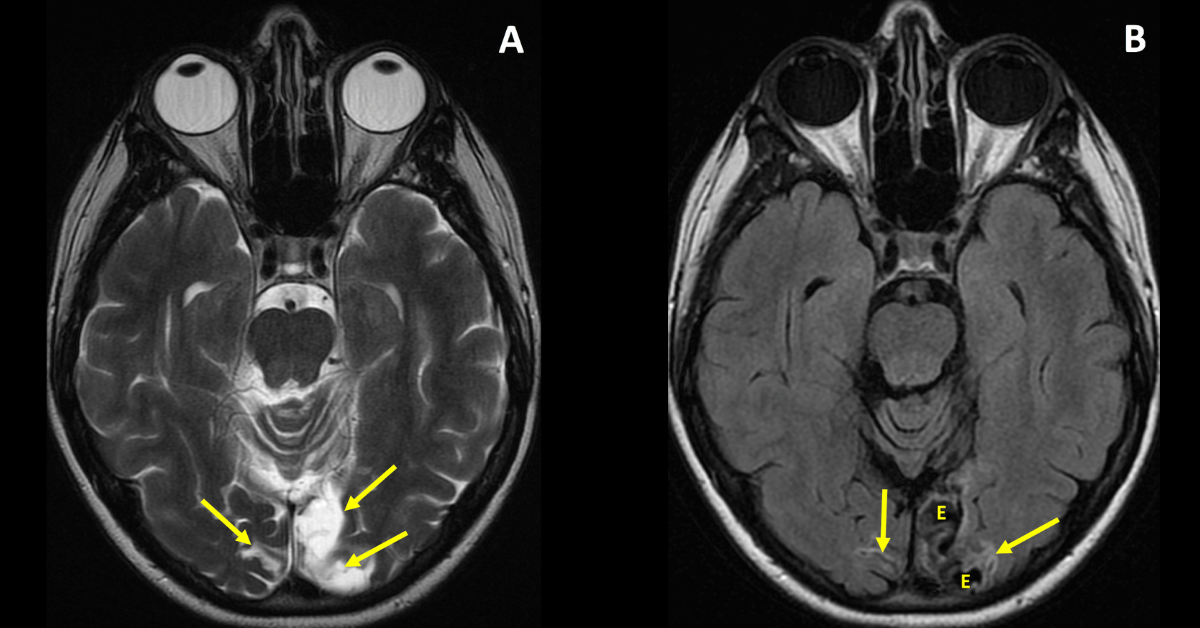
- On imaging, it shows CSF-like signal, volume loss, and negative mass effect
What Is a Encephalomalacia?
Encephalomalacia, which literally means “softening of the brain,” is a radiologic finding that often raises critical diagnostic and prognostic questions. Whether you’re a radiology resident honing your interpretive skills or a seasoned radiologist reviewing complex neuroimaging, understanding encephalomalacia is essential for clinical accuracy and confident reporting.
Definition and Pathophysiology
Encephalomalacia is a nonspecific term used to describe the end result of liquefactive necrosis of brain parenchyma. It can be focal or diffuse, and it is not limited by age, it can be observed in adults, children, and even in utero. This softening represents irreversible damage to brain tissue, which is eventually replaced by cerebrospinal fluid (CSF).
The condition can occur in any region of the brain, but after trauma, characteristic locations include the anteroinferior frontal lobes and temporal lobes.
What Causes Encephalomalacia?
The most common causes of encephalomalacia include:
Ischemic stroke (chronic infarct)
Traumatic brain injury
Intracranial hemorrhage
Infections such as encephalitis or abscess
Surgical resection or radiation necrosis
In pediatric patients, it may also result from perinatal hypoxic-ischemic injury or congenital anomalies.
What’s the Clinical Significance of Encephalomalacia?
Encephalomalacia can be an incidental finding or correlate directly with neurologic symptoms such as:
Seizures
Cognitive decline
Motor or sensory deficits
Behavioral changes
The location and extent of the lesion often influence clinical presentation and guide management decisions.
How Should Radiologists Report Encephalomalacia?
When encephalomalacia is identified, radiologists should describe:
Location and size of the lesion
Associated findings such as gliosis, hemosiderin deposition, or midline shift
Possible etiology, especially if signs of prior infarct, trauma, or hemorrhage are present
Impact on adjacent structures (e.g., mass effect, ventricular distortion)
This context helps referring physicians determine if further workup, neurologic referral, or supportive care is required.
Learn More and Review Diagnostic Cases
At Medality, we help radiologists and trainees sharpen their diagnostic accuracy with real-world cases and expert-led reviews. Our Encephalomalacia diagnosis page includes:
- Clinical imaging examples
- Case-based learning
- Tips for identifying encephalomalacia