Diagnosis Definition
- Arteriovenous malformations (AVMs) are a category of rare congenital cerebrovascular malformations
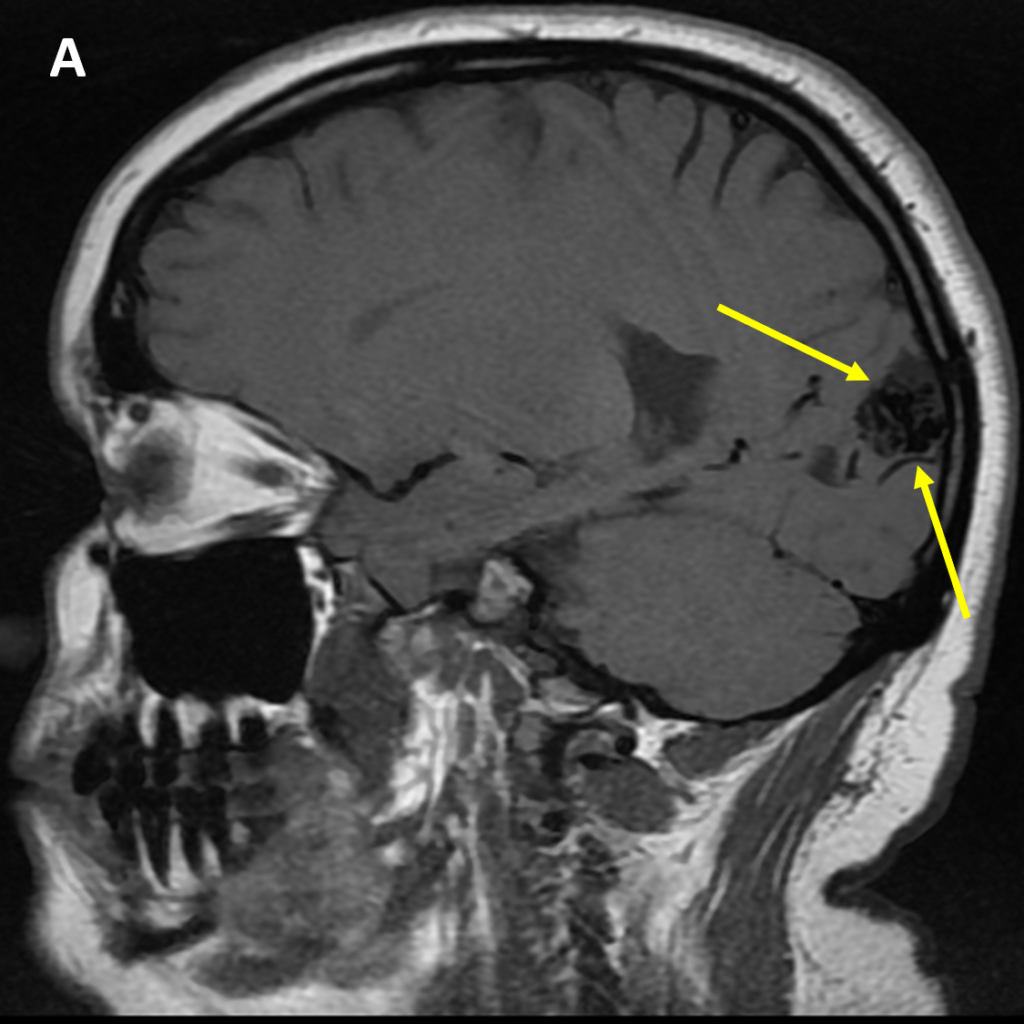
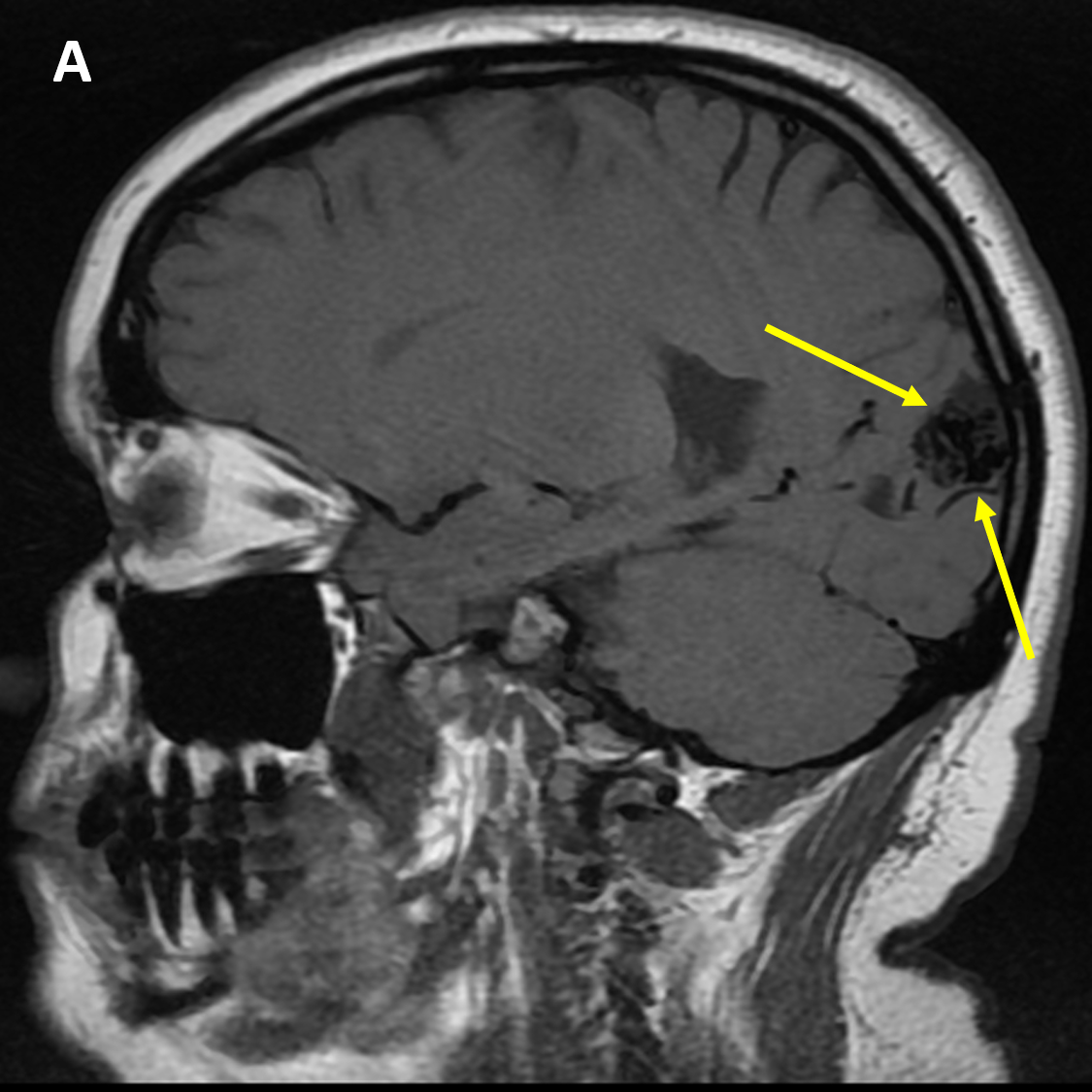
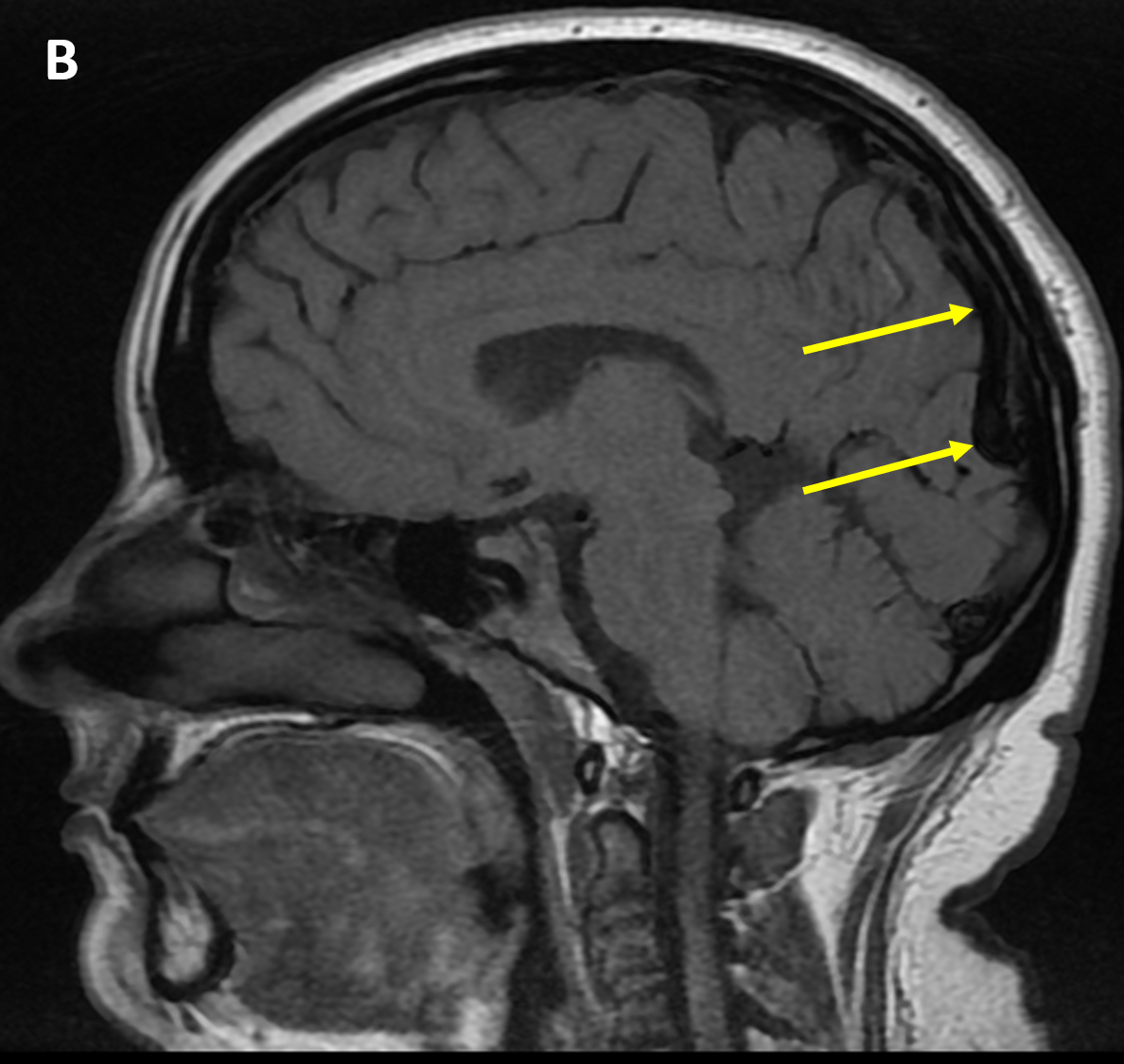
- AVMs are located in the brain parenchyma and characterized by a tangle of vessels fed by one or multiple arteries and usually drained by numerous veins
- The abnormal dilated vessels form a nidus that lacks a capillary bed, resulting in arteriovenous shunting
- The most common presenting sign is hemorrhage, followed by seizures or headaches; the risk of bleeding is 2-3% per year and AVMs are the most common cause of atraumatic parenchymal hemorrhage in young adults
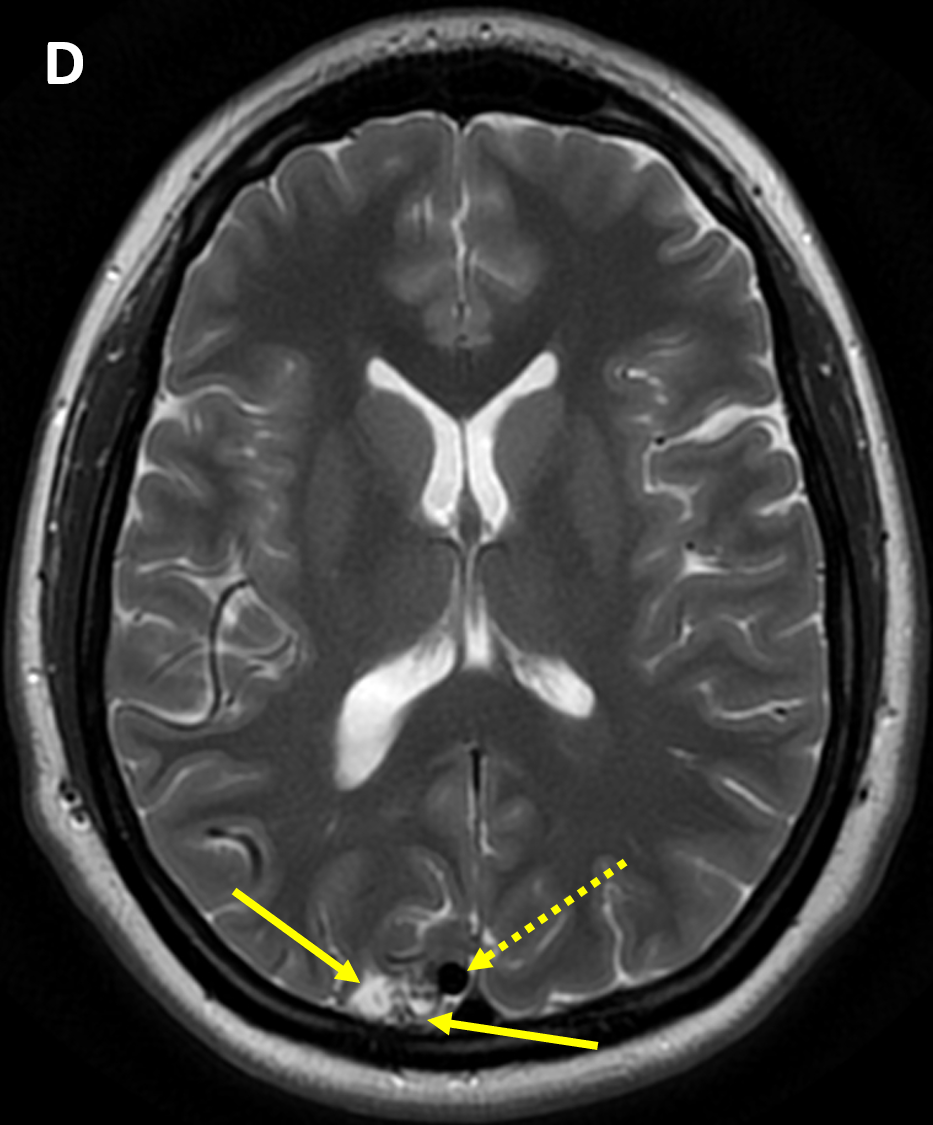
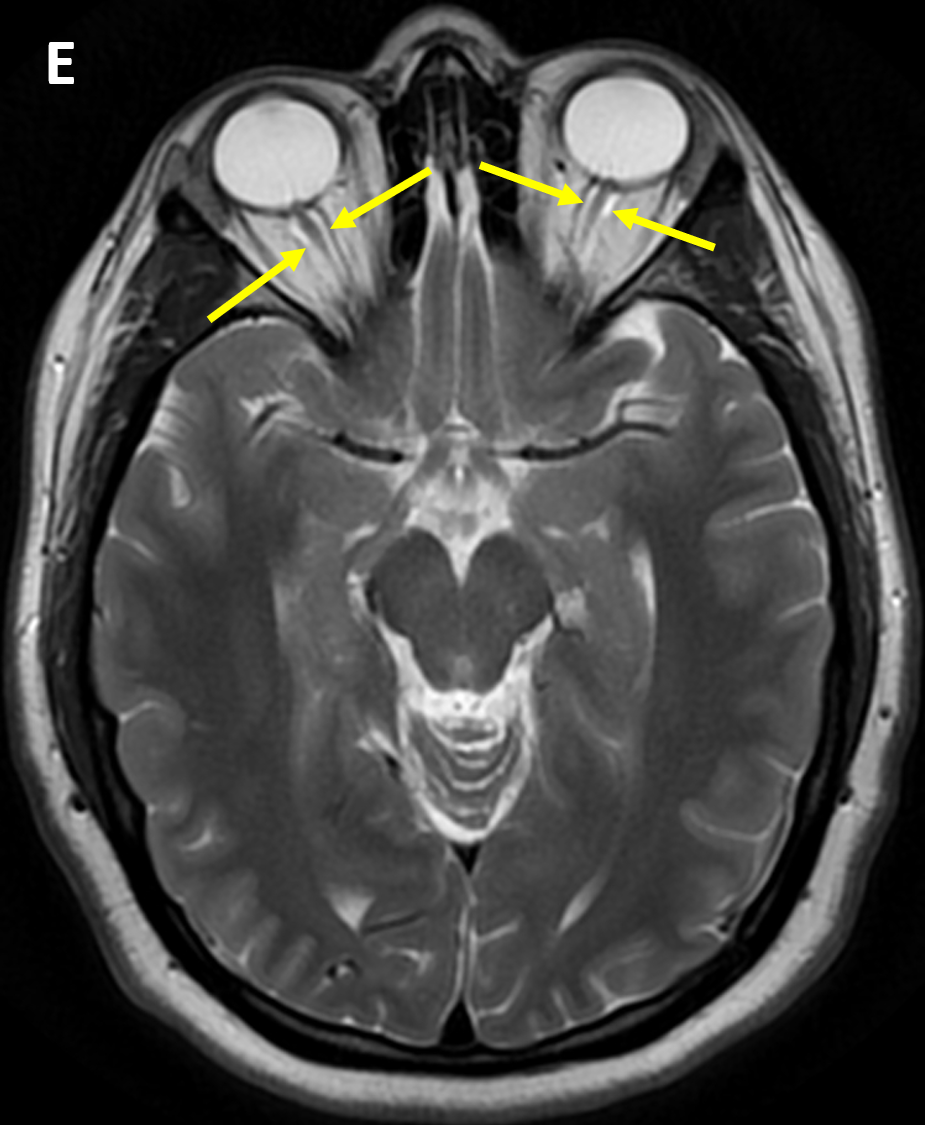
Imaging Findings
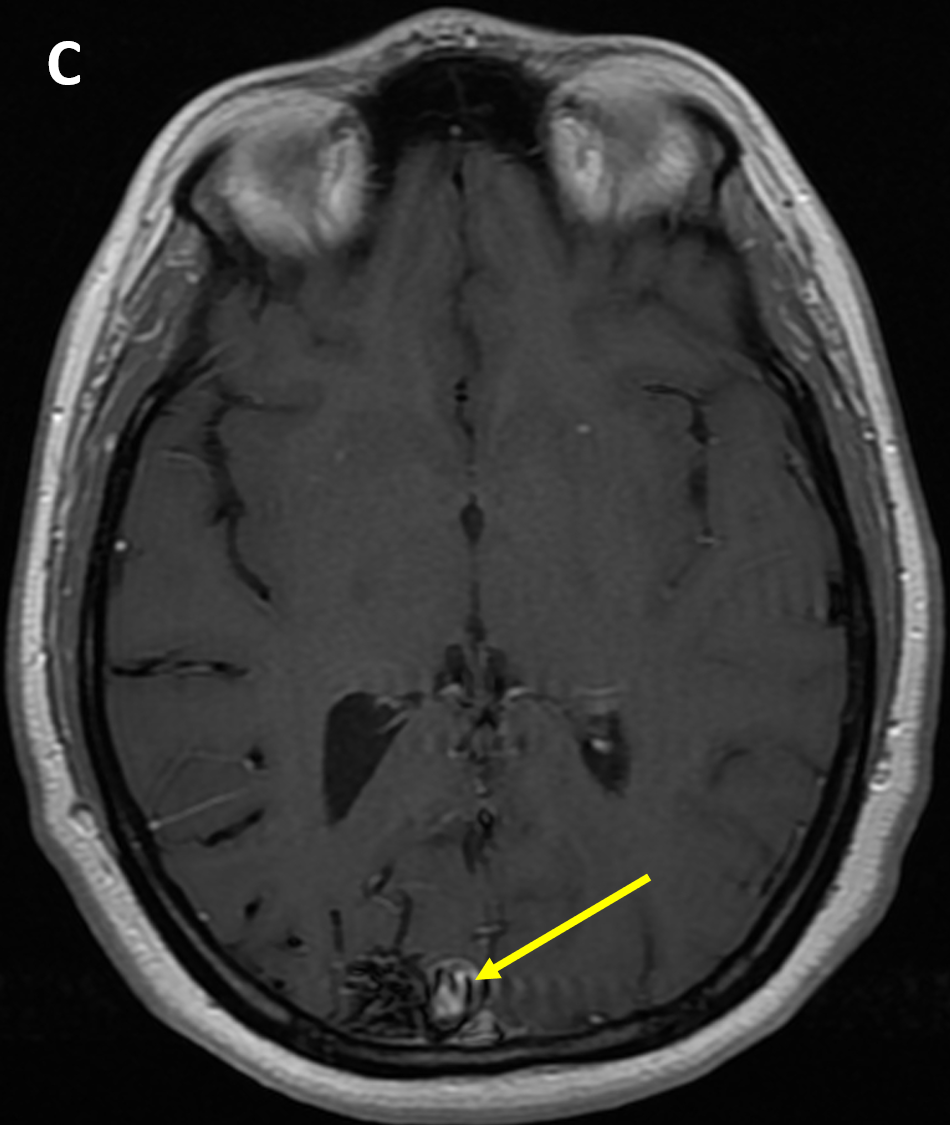
- CT scans of AVMs can show hyperdense hemorrhage or calcifications, if present, and hyperdense dilated/tortuous vessels and dominant draining vein
- MRI/MRA can identify feeding arteries and determine the location and size of the nidus, pattern of venous drainage, associated presence of aneurysms, and obstruction of venous flow
- The risk of surgical treatment of AVMs is based on the Spetzler-Martin scale, including 1) size (small <3 cm, 1; medium 3-6 cm, 2; large >6 cm, 3), 2) location (noneloquent site 0, eloquent site 1), and 3) venous drainage (superficial 0, deep 1)
Pearls
- AVMs are solitary in 98% of patients; multiple AVMs can be seen in hereditary hemorrhagic telangiectasia (aka Osler-Weber-Rendu syndrome)
- Characteristics associated with increased risk of hemorrhage include 1) prior hemorrhage, 2) presence of aneurysms, 3) drainage into deep venous sinuses, 4) venous stenosis/ectasia or single draining vein, and 5) deep location (e.g., basal ganglia, internal capsule, thalamus, or corpus callosum)
- Secondary effects of brain AVMs that may lead to nonhemorrhagic neurologic deficits include venous congestion, gliosis, hydrocephalus, or arterial steal
- Effectiveness of radiation therapy varies by AVM nidus size: 80% success rate at 3 years for AVMs that are 3cm or smaller; 30-60% if > 3 cm
References
- Geibprasert S, Pongpech S, Jiarakongmun P, Shroff MM, Armstrong DC, Krings T. Radiologic Assessment of Brain Arteriovenous Malformations: What Clinicians Need to Know. RadioGraphics 2010; 30:483–501
Case-based learning.
Perfected.
Learn from world renowned radiologists anytime, anywhere and practice on real, high-yield cases with Medality membership.
- 100+ Mastery Series video courses
- 4,000+ High-yield cases with fully scrollable DICOMs
- 500+ Expert case reviews
- Unlimited CME & CPD hours