Diagnosis Definition
- Most people have two superior and two inferior parathyroid glands, variable in location, but most commonly perithyroidal; because they measure 5 mm or less in size, normal glands are not usually seen at imaging
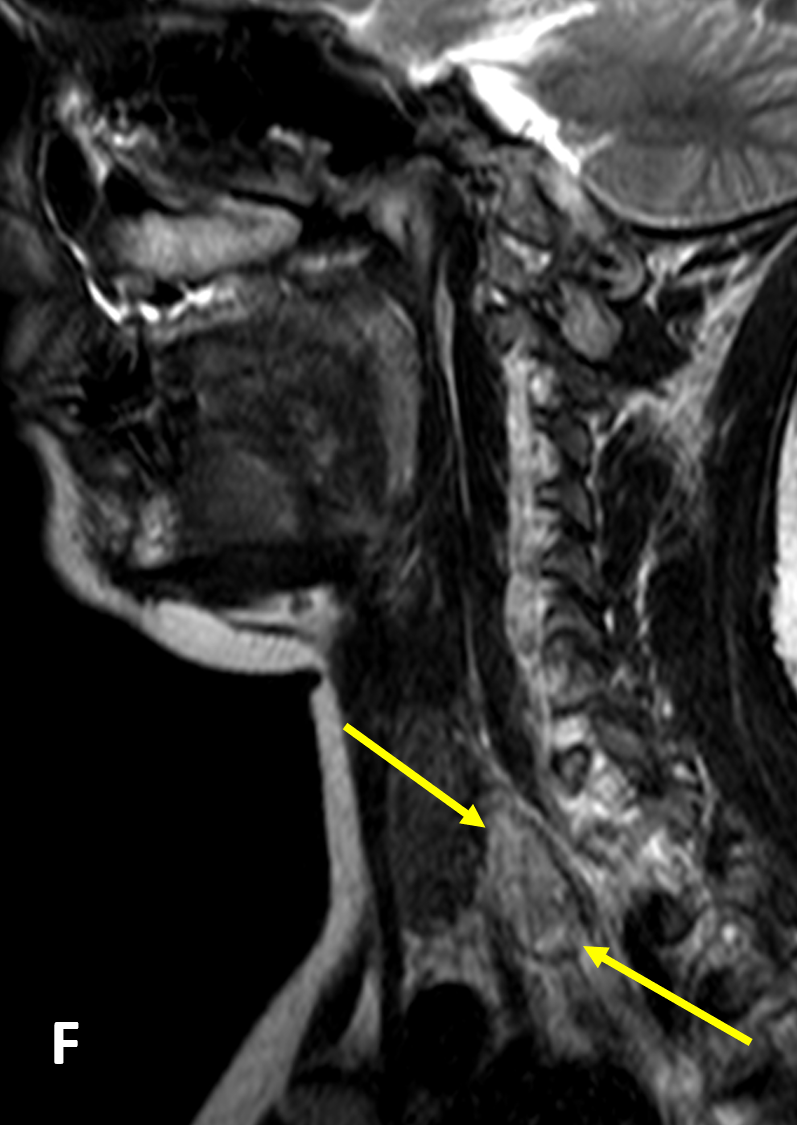
- Inferior parathyroid glands are the most variable in location; they are most commonly seen near the lower thyroid pole, but ectopically they can be located inferiorly in the neck or anterior mediastinum
- Parathyroid adenoma is the most common cause of primary hyperparathyroidism; less common causes are gland hyperplasia, multiple parathyroid adenomas, and parathyroid carcinoma
Imaging Findings
- Nuclear scintigraphy shows thallium or Technetium sestamibi accumulation within both thyroid and parathyroid tissue, and subtracted from radionuclides concentrated only in the thyroid (technetium and iodine), yields images of abnormal parathyroid tissue; alternatively, initial and delayed images using only sestamibi show initial uptake in both thyroid and parathyroid glands and retained radiopharmaceutical only within abnormal parathyroid tissue on delayed images
- Ultrasound reliably detects local adenomas (well-circumscribed oval lesions, hypoechoic to thyroid, with vascular flow) but is less accurate in detecting ectopic glands
- On CT, parathyroid tissue demonstrates rapid contrast uptake in the arterial phase and rapid washout in the venous phase, whereas lymph nodes demonstrate progressive increased uptake over the two phases; thyroid lesions are distinguished from parathyroid adenomas by being hyperdense on non-contrast CT
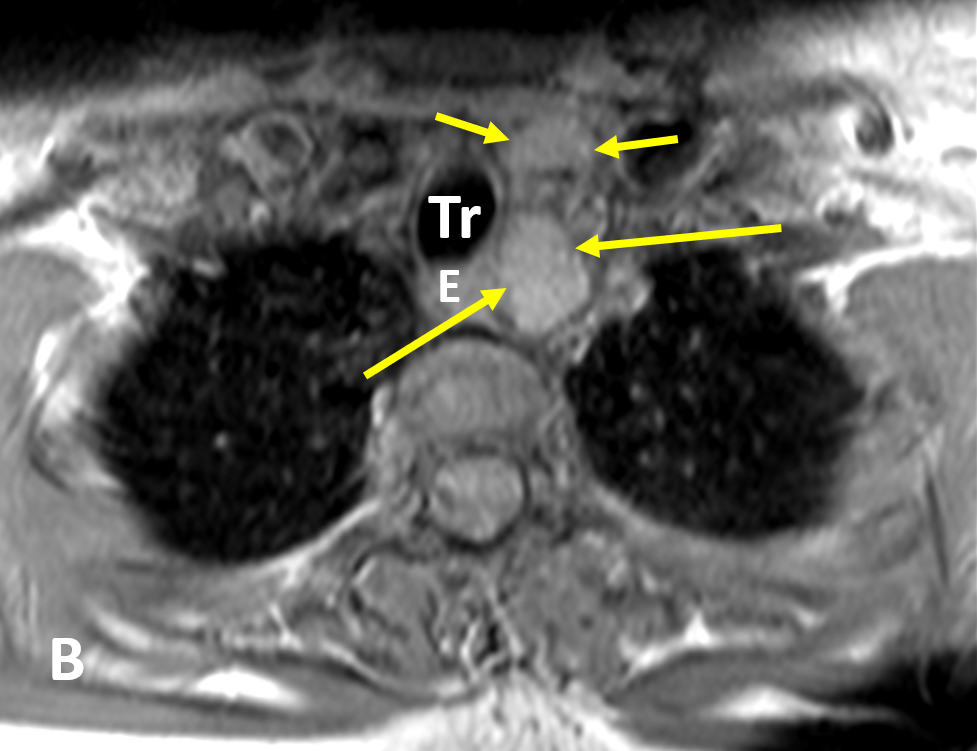
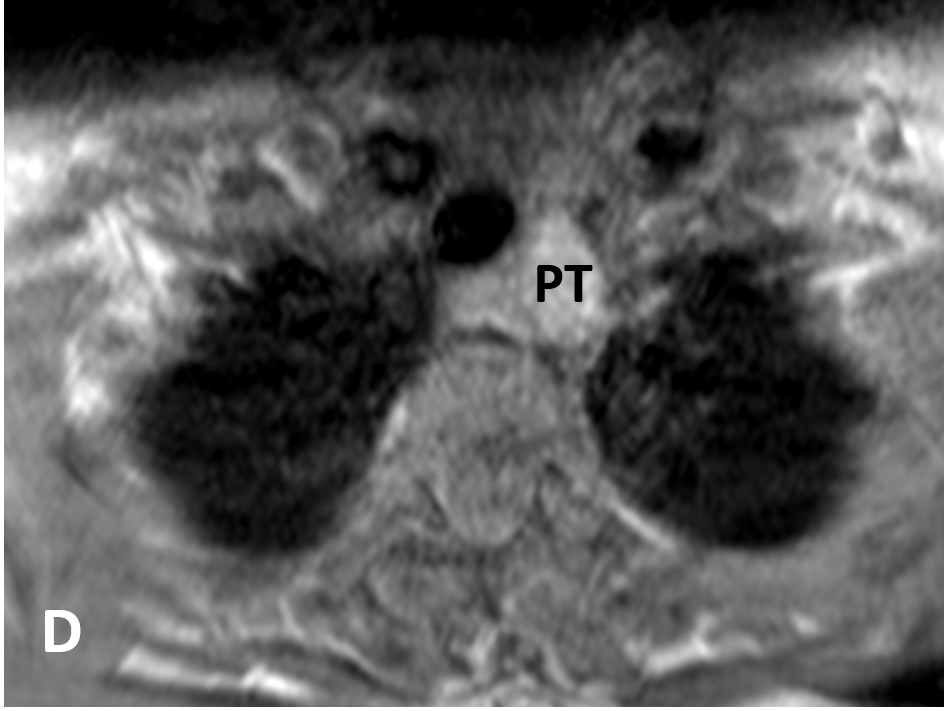
- On MRI, adenomas are usually isointense to hypointense on T1-weighted images, hyperintense on T2, and avidly enhance
Pearls
- Abnormal parathyroid tissue can have a similar appearance to lymph nodes on routine MRI; multiparametric MR perfusion can reliably distinguish parathyroid adenomas from subjacent thyroid tissue or lymph nodes
- Fibrosis or old hemorrhage within adenomas can cause low signal intensity on T1- and T2-weighted images; subacute hemorrhage into adenomas can cause high signal intensity on both T1- and T2-weighted images
References
- Gotway MB, Reddy GP, Webb WR, et al. Comparison between MR imaging and 99mTc MIBI scintigraphy in the evaluation of recurrent of persistent hyperparathyroidism. Radiology 2001; 218:783–90
- Nael K, Hur J, Bauer A, Khan R, Sepahdari A, et al. Dynamic 4D MRI for Characterization of Parathyroid Adenomas: Multiparametric Analysis. American Journal of Neuroradiology 2015; 36(11):2147-2152
- Johnson NA, Tublin ME, Ogilvie JB. Parathyroid Imaging: Technique and Role in the Preoperative Evaluation of Primary Hyperparathyroidism. American Journal of Roentgenology 2007; 188:1706-1715
Case-based learning.
Perfected.
Learn from world renowned radiologists anytime, anywhere and practice on real, high-yield cases with Medality membership.
- 100+ Mastery Series video courses
- 4,000+ High-yield cases with fully scrollable DICOMs
- 500+ Expert case reviews
- Unlimited CME & CPD hours