Diagnosis Definition
- Skull fractures can be linear/non-displaced (most common), sutural diastasis (affecting newborns and infants), depressed (inward or outward), comminuted (multiple fragments), burst (variant of comminuted, typically associated with vertebral trauma), or open/compound (communicates with air)
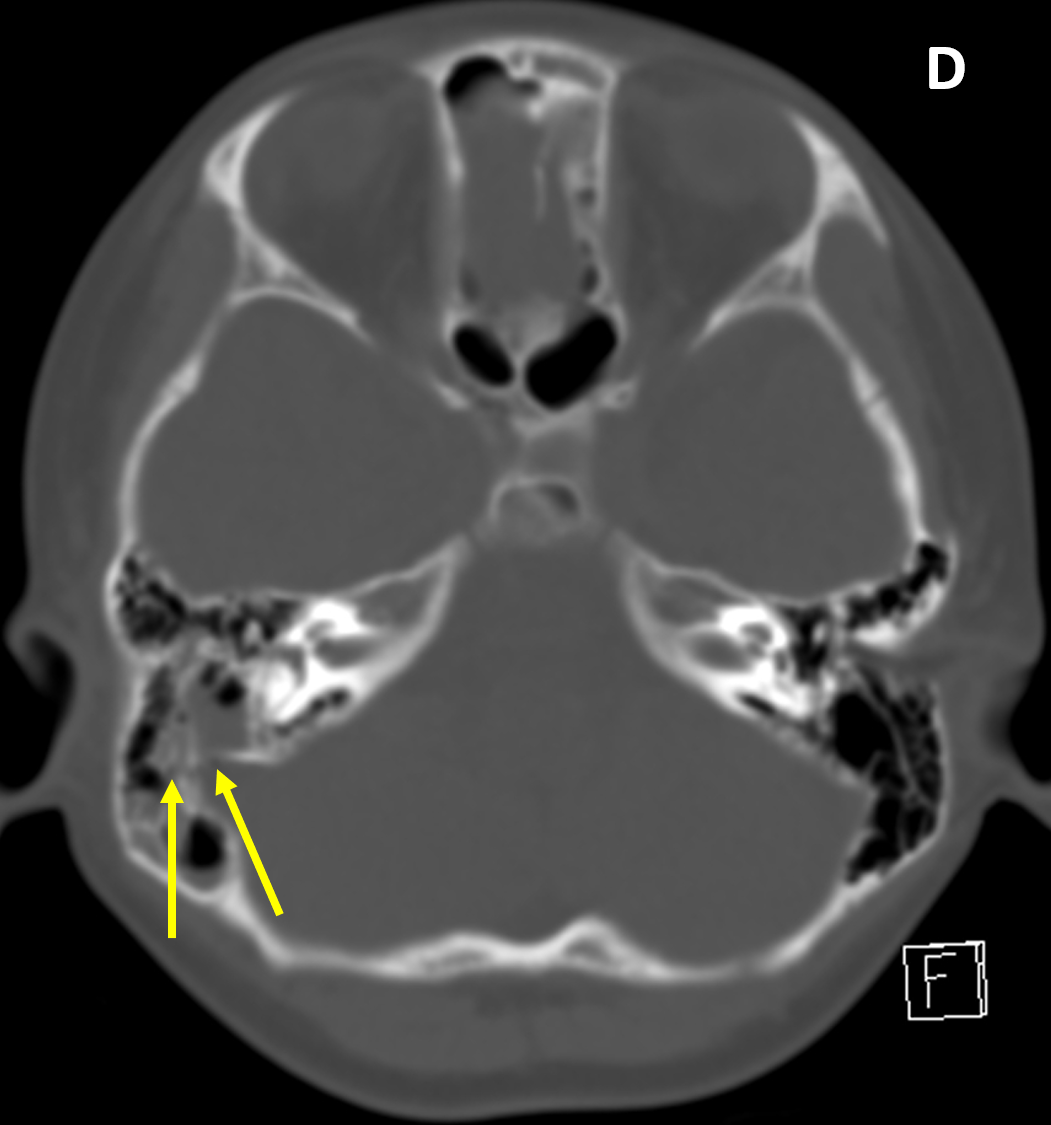
- Fractures involving paranasal sinuses or temporal bone air cells are potential sites of intracranial communication and a route of infection, cerebrospinal fluid leak (rhinorrhea, otorrhea), or pneumocephalus
- Skull fractures in infants can represent nonaccidental trauma, classically seen in an infant about 6 months old with retinal hemorrhages, subdural hematoma, and absent/minimal signs of external trauma
Imaging Findings
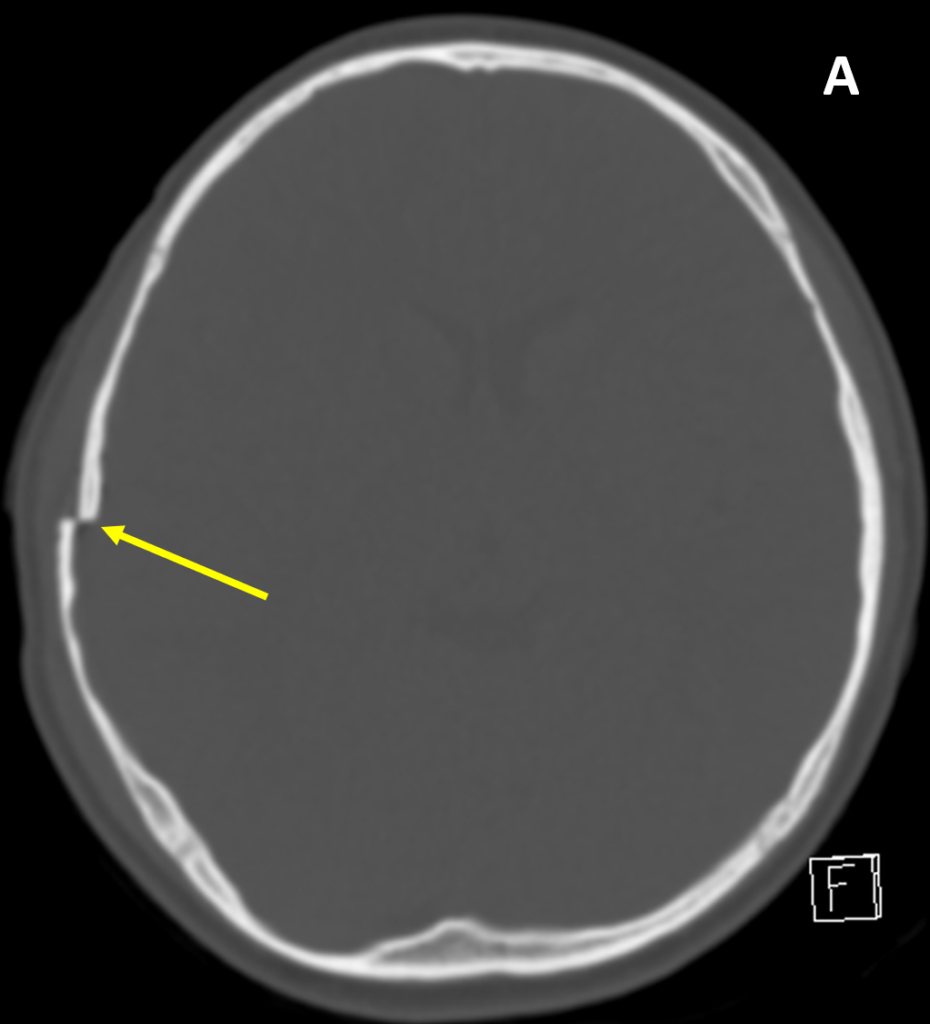
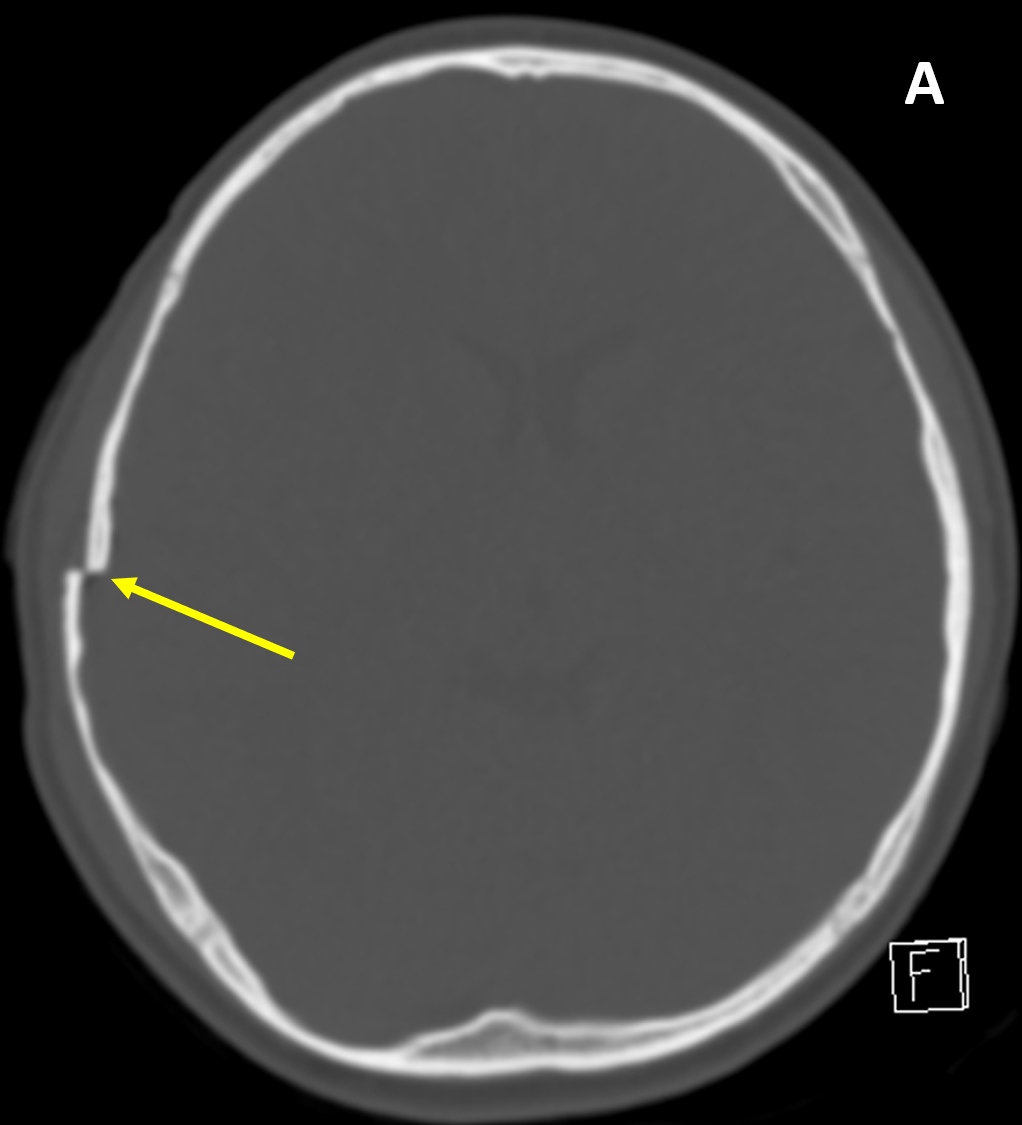
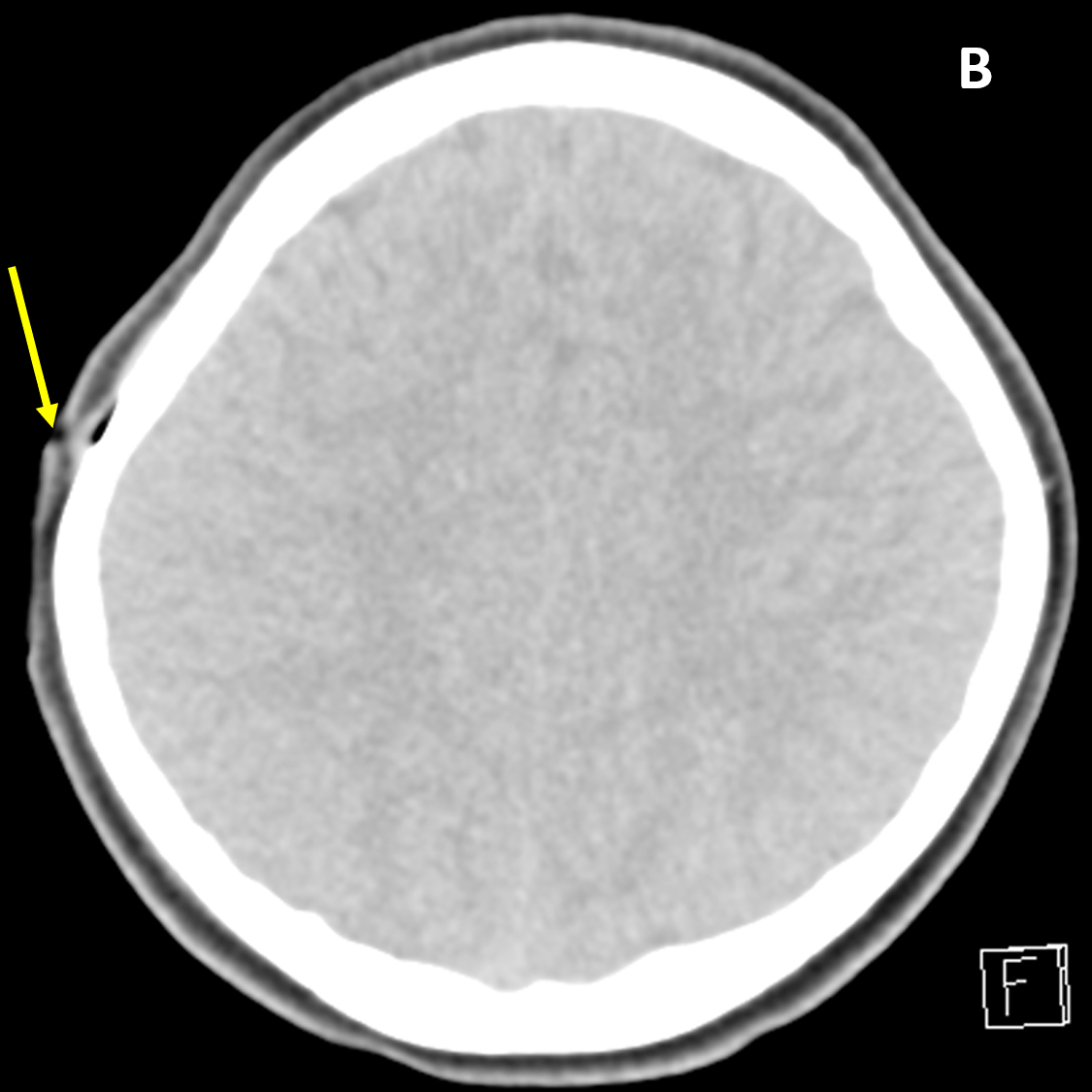
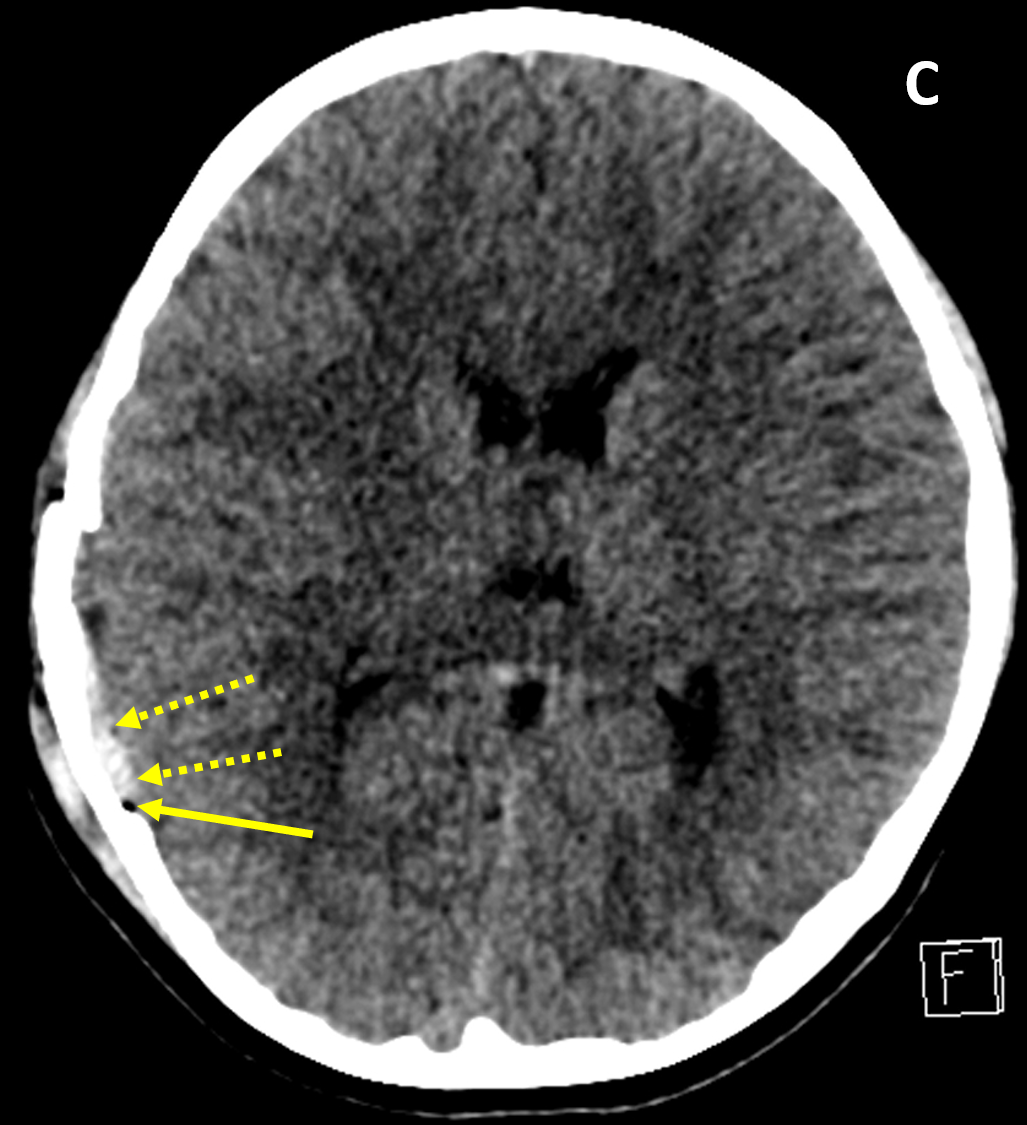
- CT better defines bone fractures than MRI and can also screen for intracranial traumatic injury (e.g., hemorrhage, herniation, hydrocephalus)
- CT window level/width should be adjusted to assess for different types of injury: 1) wide soft tissue window for scalp injury/site of impact, pneumocephalus, and extra-axial hematoma, 2) bone algorithm/window for skull fracture, and 3) brain window to evaluate for brain contusion/shearing injuries, ventricular/cisternal blood, and cistern effacement and herniation
- MRI can be used to evaluate associated non-bony injury and is particularly useful in cases of new or deteriorating cognitive or neurologic deficits, delayed recovery, or persistent unexplained deficits; it is more sensitive than CT for skull base hematomas and shearing injuries
Pearls
- Presence of a scalp injury should prompt a search for an associated skull fracture
- Fractures with fragment depression greater than the adjacent inner table may require surgical elevation
- Vascular grooves/channels are differentiated from fractures by having a branching pattern, appearing wavy rather than sharp and straight, tapering, and showing symmetry with the opposite side
- In the setting of trauma and opacified mastoid air cells, a temporal bone fracture should be assumed until proven otherwise
References
- Shetty VS, Reis MN, Aulino JM, Berger KL, Broder J, et al. ACR Appropriateness Criteria Head Trauma. J Am Coll Radiol 2016; 13(6):668-679
- Zayas JO, Feliciano YZ, Hadley CR, Gomez AA, Vidal JA. Temporal Bone Trauma and the Role of Multidetector CT in the Emergency Department. RadioGraphics 2011; 31:1741–1755
Case-based learning.
Perfected.
Learn from world renowned radiologists anytime, anywhere and practice on real, high-yield cases with Medality membership.
- 100+ Mastery Series video courses
- 4,000+ High-yield cases with fully scrollable DICOMs
- 500+ Expert case reviews
- Unlimited CME & CPD hours