Diagnosis Definition
- Spinal epidural abscess (SEA) is an infection of the epidural space, located between the spinal dura mater and the vertebral periosteum
- Diabetes and intravenous drug use are the most significant risk factors for SEA
- Symptomatic patients most commonly present with back pain, fever, and severe focal tenderness
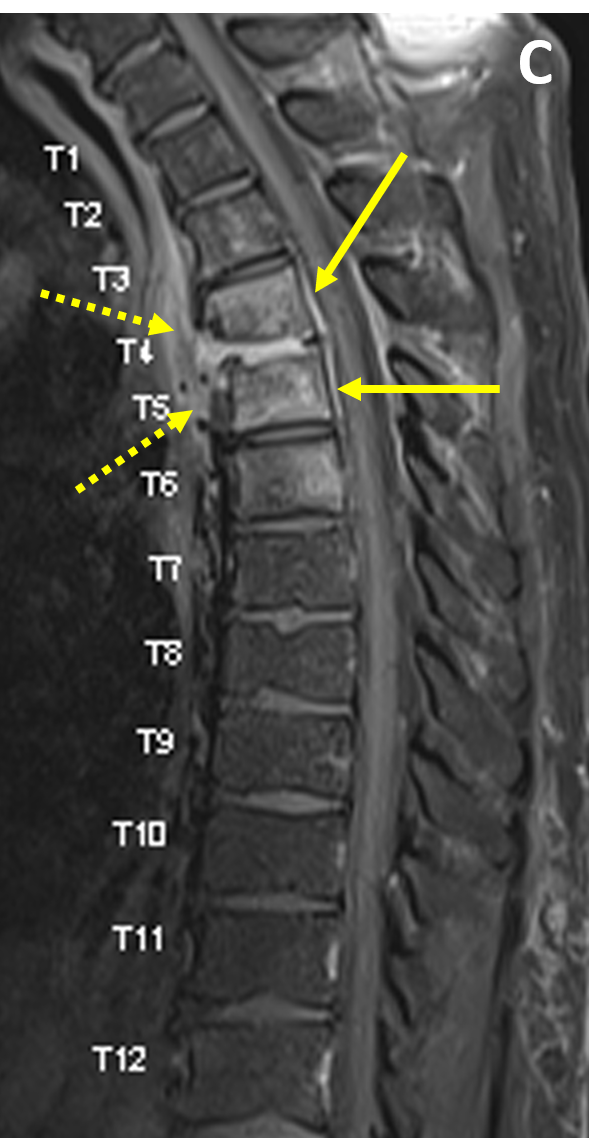
- SEA most often results from 1) hematogenous dissemination of microbes from a remote infection, 2) contiguous spread of infection, such as from adjacent vertebral discitis-osteomyelitis (VDO), or 3) direct inoculation, such as from penetrating trauma, discography/biopsy/other surgical procedures, and spinal anesthesia
Imaging Findings
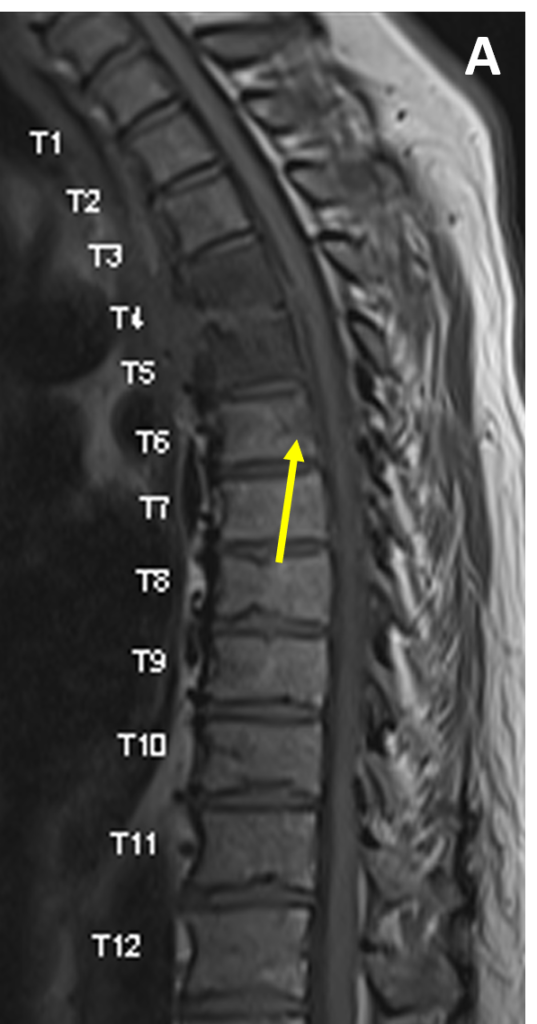
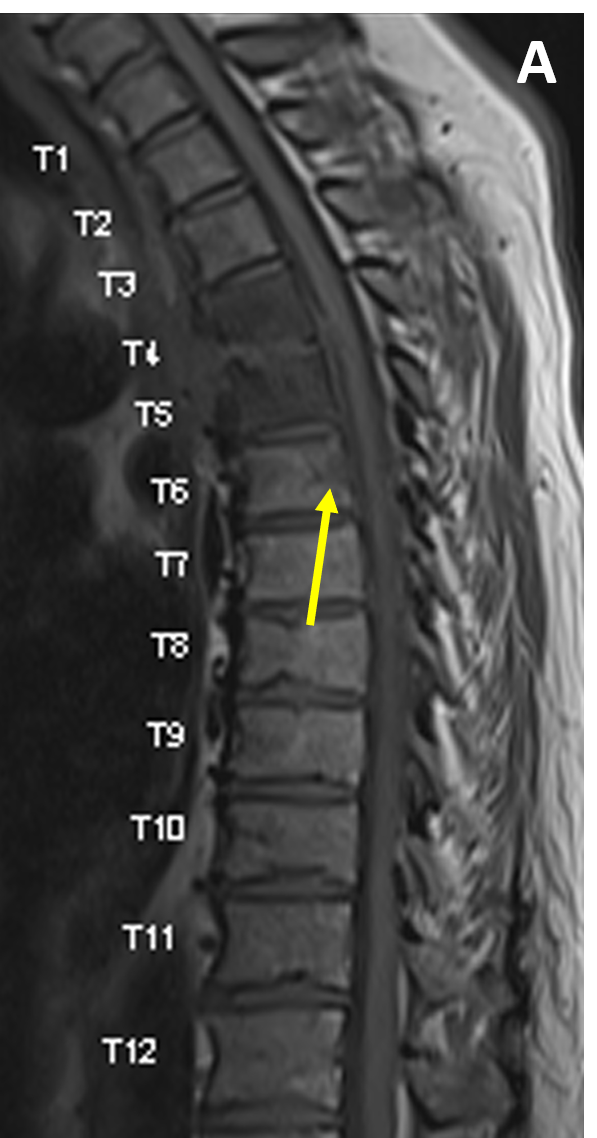
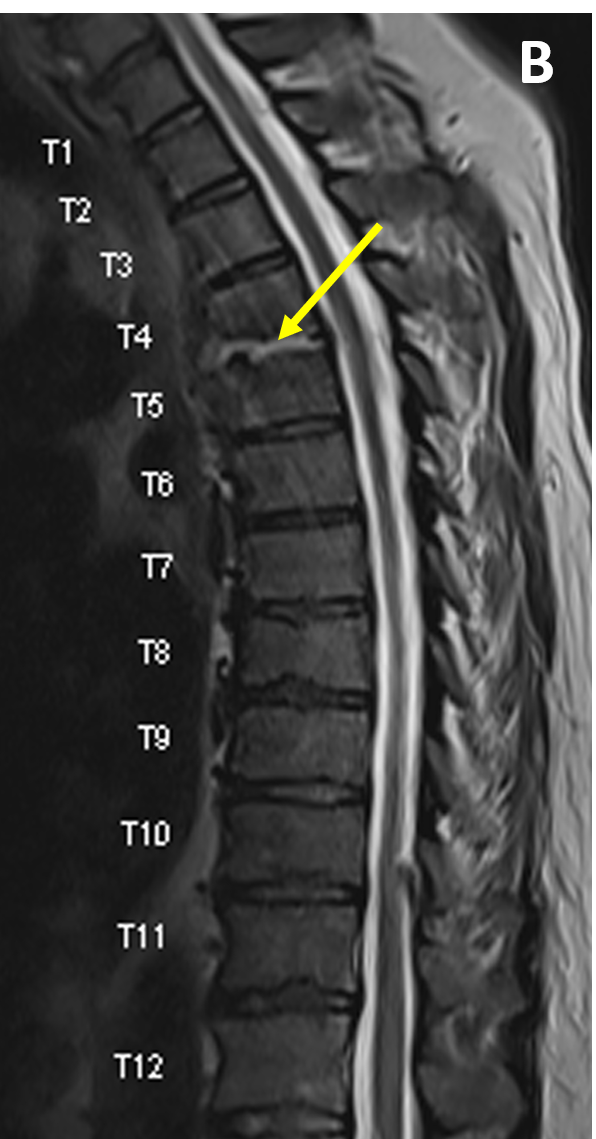
- MRI is 91% – 100% sensitive for SEA, most often showing a soft tissue mass with tapering edges in the spinal epidural space with mass effect on the thecal sac and spinal cord
- SEA appears isointense to the spinal cord on T1-weighted images and hyperintense to cord on T2/ STIR scans
- Postcontrast enhancement can be thin and peripheral, heterogeneous, or diffuse and smooth
- Bright signal on diffusion-weighted imaging (DWI), confirmed by low values on apparent diffusion coefficient (ADC) mapping within the abscess represents abnormal restricted diffusion, a feature of SEA
- A low signal area on T1 that is high signal on T2 and shows no central area of enhancement is consistent with a liquid abscess that is amenable to surgical drainage
Pearls
- SEA can appear similar to a phlegmon; the distinction is critical as SEA often requires surgical treatment
- Paralysis, which can result from spinal compression or ischemia secondary to septic thrombosis, requires urgent intervention
- Differential diagnostic considerations include vertebral metastases (with extradural extension), epidural hematoma, extruded or migrated lumbar disc, and postoperative spinal seroma
References
- Laur O, Mandell JC, Titelbaum DS, Cho C, Smith SE, Khurana B. Acute nontraumatic back pain: infections and mimics. RadioGraphics. 2019; 39(1): 287-288
- Reihsaus E, Waldbaur H, Seeling W. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev. 2001; 23(4):175-204
Case-based learning.
Perfected.
Learn from world renowned radiologists anytime, anywhere and practice on real, high-yield cases with Medality membership.
- 100+ Mastery Series video courses
- 4,000+ High-yield cases with fully scrollable DICOMs
- 500+ Expert case reviews
- Unlimited CME & CPD hours